A Complete Guide to Wound Dressing
Wound management can be an overwhelming practice for nurses, first responders, clinicians, and anyone who needs to protect and treat an injury. From advanced wound dressing to wound dressing at home, choosing the right dressing can significantly cut down healing time, make a patient considerably more comfortable, and fight off risks like infection and complications further down the line.
This is our complete wound dressing guide, covering all the basic essentials of wound dressing.
Wounds and Dressings: How to Select the Right Dressing
Primarily, consider the following when choosing a wound dressing.
- The size of the wound area
- The depth of the wound
- How much exudate the wound is producing
- The location of the wound on the body
There are also some patient and lifestyle-related factors that rely on the characteristics of wound dressing. Is the patient in a lot of pain or distressed? How often will the dressing need to be changed? Who will change the dressing, a nurse or an untrained person?
A simple wound dressing must usually be in direct contact with a wound, so it's also important to consider how well it will conform to the specific area of the body to which it's applied. Will the dressing be in a joint crevice and so need to be flexible and malleable? Will it be on the heel of the foot, and so need to be minimally bulky?
It’s also important to be aware of the way a wound changes over time as it heals. For example, a dressing must be selected based on the level of exudate a wound produces. Ideally, the dressing should absorb enough exudate to avoid skin maceration but not so much that it dries out the wound bed and causes the healing process to slow down or even put the wound at risk of infection. You may need to opt for a breathable wound dressing or a moist wound healing dressing, depending on the state of the wound.
Some wound dressings are so effective that they cause over-granulation due to an over-activated wound bed which prevents the top layer of skin from healing over the wound. Care and observation must be taken to ensure the dressing meets the changing needs of the wound.
Refer to the table below to check which dressings best suit the wound conditions.
Find out exactly what is in an animal first aid kit from Steroplast along with when each item can be used:
| Dressing Type | Primary/Secondary | Level of Exudate | Change Frequency | Wound Depth |
|---|---|---|---|---|
| Alginate | Primary | Moderate to heavy | Daily | Deep |
| Collagen | Primary | Minimal to moderate | Daily | Mid to deep |
| Composite | Primary/secondary | Moderate to heavy | 3 x per week | Mid to deep |
| Foam | Primary/secondary | Moderate to heavy | 3 x per week | Deep |
| Gauze | Primary/secondary | Minimal to heavy | Daily or down to 3 x per week | Mid to deep |
| Hydrocolloid | Primary/secondary | Minimal to moderate | 3 x per week | Mid to deep |
| Hydrogel | Primary/secondary | Minimal | Daily or down to 3 x per week | Deep |
| Transparent | Primary/secondary | Minimal to moderate | 3 x per week | Closed to mid |
| Wound Packing | Primary | Minimal to heavy | Daily | Mid to deep |
Find out exactly what is in an animal first aid kit from Steroplast along with when each item can be used:
| Dressing Type | Alginate |
|---|---|
| Primary/Secondary | Primary |
| Level of Exudate | Moderate to heavy |
| Change Frequency | Daily |
| Wound Depth | Deep |
| Dressing Type | Collagen |
| Primary/Secondary | Primary |
| Level of Exudate | Minimal to moderate |
| Change Frequency | Daily |
| Wound Depth | Mid to deep |
| Dressing Type | Composite |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Moderate to heavy |
| Change Frequency | 3 x per week |
| Wound Depth | Mid to deep |
| Dressing Type | Foam |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Moderate to heavy |
| Change Frequency | 3 x per week |
| Wound Depth | Deep |
| Dressing Type | Gauze |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Minimal to heavy |
| Change Frequency | Daily or down to 3 x per week |
| Wound Depth | Mid to deep |
| Dressing Type | Hydrocolloid |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Minimal to moderate |
| Change Frequency | 3 x per week |
| Wound Depth | Mid to deep |
| Dressing Type | Hydrogel |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Minimal |
| Change Frequency | Daily or down to 3 x per week |
| Wound Depth | Deep |
| Dressing Type | Transparent |
| Primary/Secondary | Primary/secondary |
| Level of Exudate | Minimal to moderate |
| Change Frequency | 3 x per week |
| Wound Depth | Closed to mid |
| Dressing Type | Wound Packing |
| Primary/Secondary | Primary |
| Level of Exudate | Minimal to heavy |
| Change Frequency | Daily |
| Wound Depth | Mid to deep |
Proper Wound Dressing
Wound dressing technique is crucial if you want a wound to heal without complications. An unsuitable dressing could lead to infection, pain, discomfort, skin maceration, over-granulation, dehydration, and many other issues. Start with the basics by reading our article What is a Wound Dressing? Find out everything you need to know about wound dressing in general.
Types of Wound Dressings
Dressing a wound starts with choosing the right type of dressing, and with so many options, care and consideration must be taken to ensure you pick a dressing that has the right level of absorption (or none at all), breathability (or none at all), and active ingredients (if any).
Here are some features of different dressing types to help you decide what to use to dress a wound.
What happens if something goes wrong? Check our guide Troubleshooting Wound Dressing: What to Do When Something Goes Wrong
Aseptic Non-Touch Technique Wound Dressing
Is wound dressing a sterile procedure? It doesn’t always have to be, but use the aseptic technique when it does. Use the aseptic technique in wound dressing to dress wounds without introducing any new bacteria or potentially infectious agents to the wound. The aseptic technique for wound dressing can be used on any wound, whether it is currently infected or not, as an excellent measure against exacerbating a wound or complicating the healing process.
You will need:
- A sterile dressing procedure pack
- A clean surface large enough to place the wound pack on. A stainless steel trolley is ideal.
- A sink with soap and water, plus wound washing solution if needed.
- Separate disposable gloves to remove the current dressing.
- A disposable apron.
- Dressings appropriate for the wound.
We cover all the equipment needed to dress a wound in our blog post Equipment Needed for Wound Dressing in case you need to check.
Follow these steps to carry out a dressing change with ANNT.
- Ensure the patient is comfortable and arrange the dressing pack close by on the clean surface.
- Wash your hands and put on the apron.
- Open the sterile field of the dressing pack using the corners.
- Arrange the items in the dressing pack on top of the sterile field. You can either use sterile forceps to do this or identify the disposable bag in the dressing pack and open it up. Put your hand in the bag and use this to arrange the items. Then invert the bag and place it close by in an area where you won’t pass soiled items across the sterile field.
- Prepare any compartment trays and wound-cleaning equipment.
- Wash your hands and put on some disposable gloves.
- Place the dressing towel under the body area being treated. Slowly lift the old dressing away and put it in the waste bag.
- Clean the dressing as necessary.
- Remove your gloves by pinching the inside edge of each at the wrist and inverting them. Put them in the waste bag and wash your hands.
- Apply the sterile gloves in the dressing pack
- Dress the wound as required, not touching any non-sterile areas or items.
- Remove the gloves and dispose of all used items in the waste bag.
- Wash your hands and disinfect surfaces.
- Dispose of the waste bag following your local or organisation’s procedures
How to Clean a Wound Before Dressing
Cleaning a wound before dressing it is important. If the wound is recent and you’re preparing to dress it for the first time, you may need to clear the wound bed of dirt, debris, stuck objects, and anything that entered the wound as a result of the injury. You should also aim to clear bacteria from the wound to reduce the chance of infection.
As the body heals, it will push bacteria and foreign debris out of the wound bed, along with exudates like pus and blood. These should be cleaned away during dressing changes so a hygienic environment is maintained and bacterial growth at the wound site is managed.
Cleaning a Wound Immediately After Injury

If something is embedded in a wound, it should only be removed by a professional. Call 999 or take the casualty to A&E if you are not a professional.
- Wash your hands and put on disposable gloves if you can.
- Rinse the wound under running water. You could hold it under a tap or pour water over the wound with a jug. You could also use normal saline solution or a saline wound wipe.
- Pat the area dry with a clean piece of gauze.
Cleaning a Wound Between Dressing Changes

If you are cleaning a wound between dressing changes, you may want to follow these steps.
- Wash your hands and put on disposable gloves.
- Carefully remove the soiled dressing by lifting it up or rolling it away. Remove the dressing in the direction of hair growth.
- Inspect the wound and tell the physician if there are signs of the wound worsening.
- Moisten gauze swabs in sterile water or sterile saline solution and wring out the excess. Do this with two pairs of sterile forceps.
- Holding a gauze swab in a pair of forceps, swipe around the wound, moving from the least contaminated areas to the most.
Gauze is an excellent material for cleaning and drying wounds because it is non-linting. That means there’s hardly any chance fibres will come away from the gauze and stick to the wound bed, making cleaning and drying a wound much easier and less uncomfortable for the patient. Learn about gauze in our article All About Gauze Swabs.
Limited-time Offers
Save £420 on Defibrillator Bundles
Shop our Bundle Discounts.
How to Get a Dressing off a Wound
When removing wound dressing materials, take care not to spread any exudate or dead tissue by moving the dressing around on the wound. The soiled dressing may harbour bacteria that could aggravate the wound or contaminate surrounding areas, so wound dressing removal should minimise the chance of transferring any of this.
Consider these things when removing a dressing from a wound:
- Have you washed your hands and put on disposable gloves?
- Is the environment clean and disinfected?
- Do you have all the materials and equipment to hand before you start?
- Do you have clean water or saline solution ready to help loosen the dressing if needed?
- Is there a clinical waste disposal bag close by that you can dispose of soiled dressing into? This bag should be place where you do not need to pass over the sterile field with soiled dressings.
How to Remove Dressing From Wound
- Wash your hands and put on disposable gloves (non-sterile).
- If there is dressing retention tape, loosen this by holding the skin beside it taught and gently pulling it away in the direction of hair growth. Loosen the tape on all sides of the dressing before lifting the dressing off the wound.
- Grasp the dressing at the corners and slowly remove it. For a long dressing, you can roll it back on itself like a bandage. You can simply lift the dressing up and off the body for square or short dressings.
- Dispose of the dressing in a waste disposal bag.
- Inspect the wound bed for dressing fibres. These can be removed carefully with tweezers if needed.
How to Remove a Dressing That Is Stuck to Wound
If you’re looking for how to get a dressing off a wound to minimise patient discomfort, you can try soaking the dressing in warm saline solution or warm, clean water. If the dressing is on an extremity, you might be able to submerge it completely. Otherwise, use a soaked cotton ball to dab the dressing.
Carefully pull the dressing away bit by bit. You may need to re-wet it a few times. Inspect the wound bed afterwards to ensure no fibres are still stuck down. This is usually the best method if you need to know how to remove dressings from wounds without pain.
For how to stop wounds sticking to dressings, ensure the wound bed is clean and dry (or dry as possible) before putting a dressing on. You may also want to opt for a low-adhesive dressing that minimises the risk of sticking down.
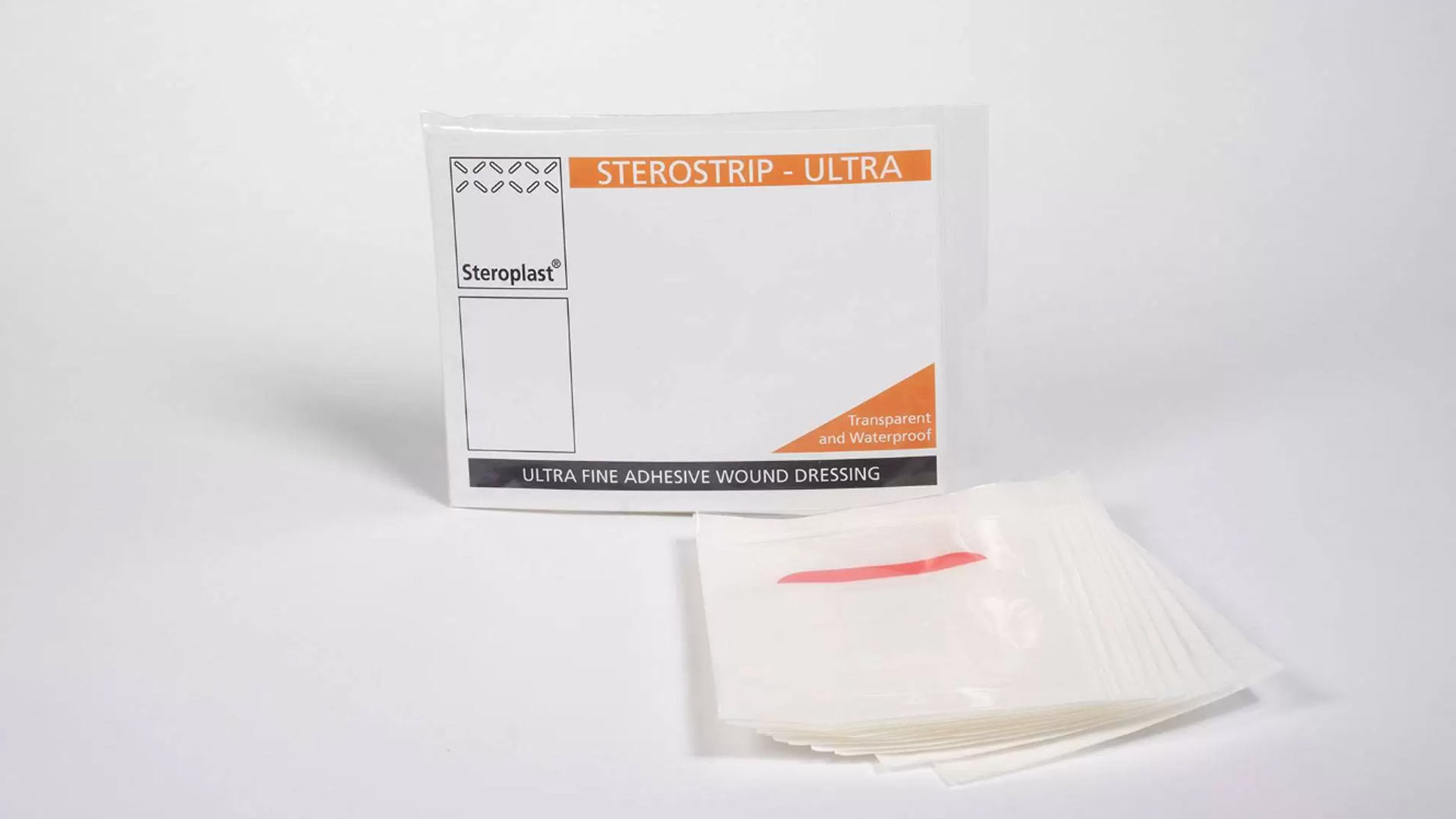
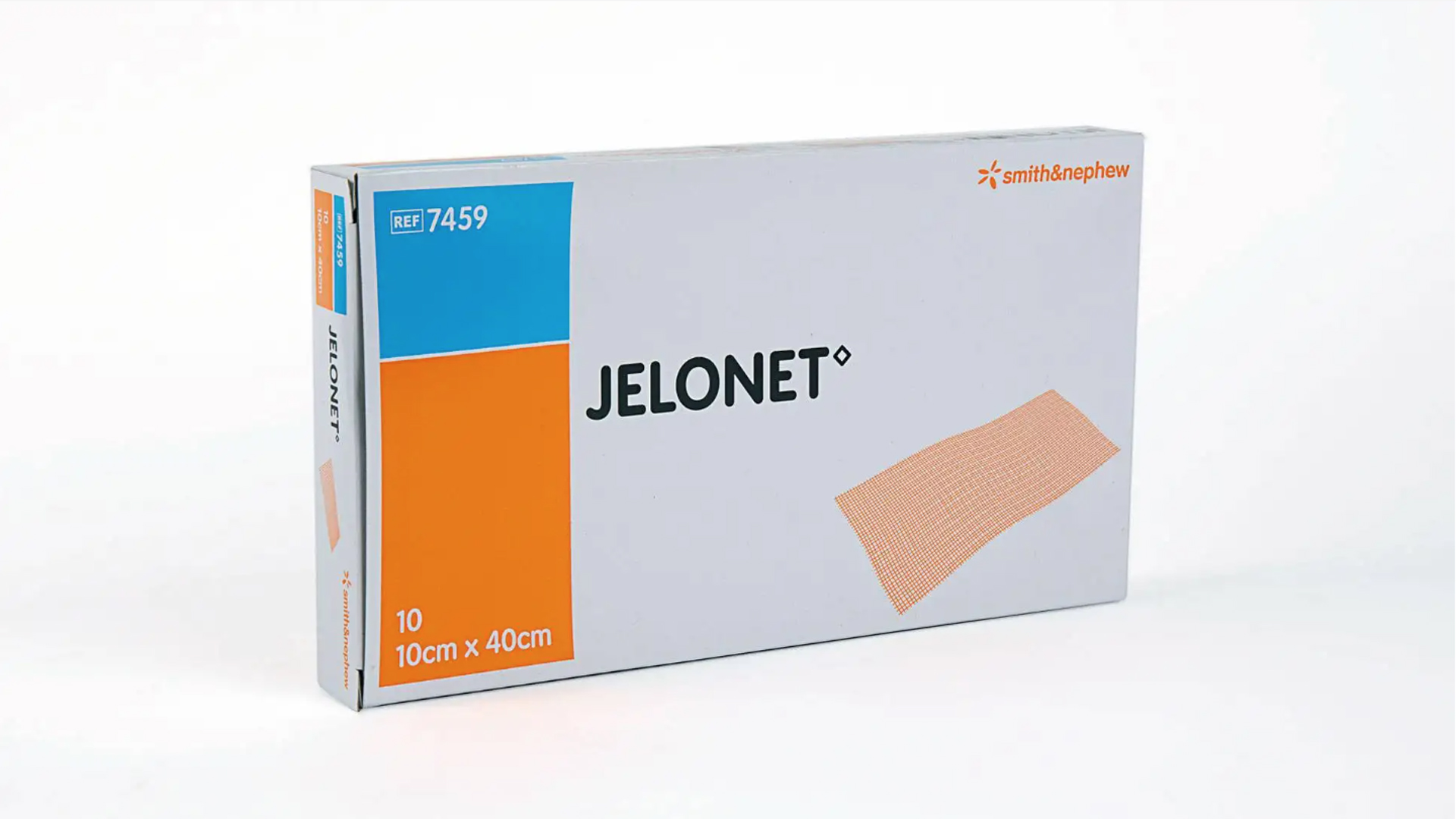
How to Dress a Wound So It Doesn’t Stick
Maintaining a moist environment will prevent a dressing from drying out and sticking to a wound. This is a recommended solution for how to dress a wound without it sticking. Gauze soaked in vaseline or paraffin is a good material to use. Jelonet is a good example of this type of dressing. It wicks exudate away from the wound, passing it to an absorbent secondary wound dressing while maintaining moisture levels, so the wound stays hydrated. Steropax is a good choice for secondary dressings for wounds.
How to Change Wound Dressing
About Wound Care and Dressing Changes
Changing a dressing on a wound helps to remove bacteria and exudate that the body pushes out of the wound bed, keeping the site as clean as possible to help the body heal and grow new tissues.
The type of dressing used will determine wound care dressing change frequency. Occlusive dressings must be changed regularly, at least once a day. Polyurethane dressings used to cover closed surgical wounds might only need to be changed every few days or not at all until they are removed completely.
Changing surgical wound dressings can generally be done less frequently because they are dry, closed wounds that shouldn’t produce exudate and pose a very minimal risk of infection.
Changing the Dressing on a Wound
Here are the steps and considerations you should consider with changing a dressing on a wound.
Visit our
Interactive First Aid Guide
Demystify workplace first aid & find out exactly what your business needs.
Please enter your details into the form below along with any questions or comments and a member of our team will be happy to provide you with more information: